Inflammation
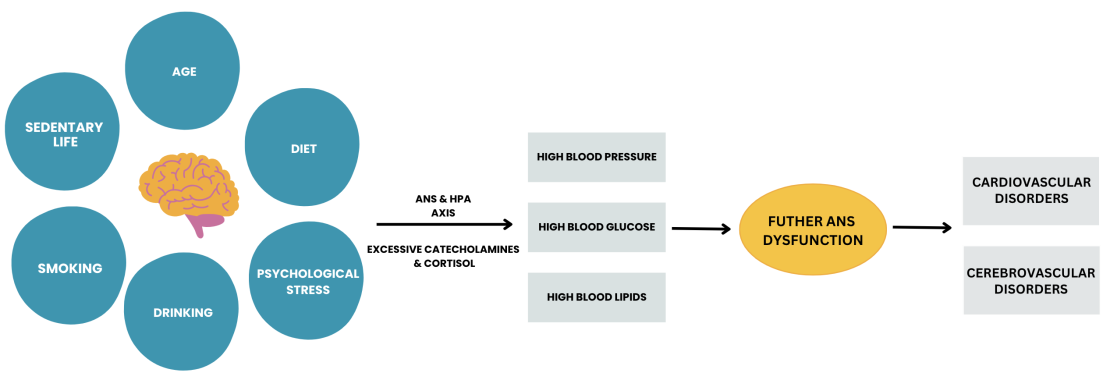
The The body’s immune system also responds to threats, such as infection, physical injury, emotional or mental insult with a cascade of changes that lead to localised inflammation.The immune system recognizes and attempts to remove harmful stimuli and begins the healing process.This is the proposed process of acute stress.
These states are beneficial to our survival and recovery. However if the stress exposure is continuous, chronic stress is the outcome.Chronic stress result failures of homeostasis.
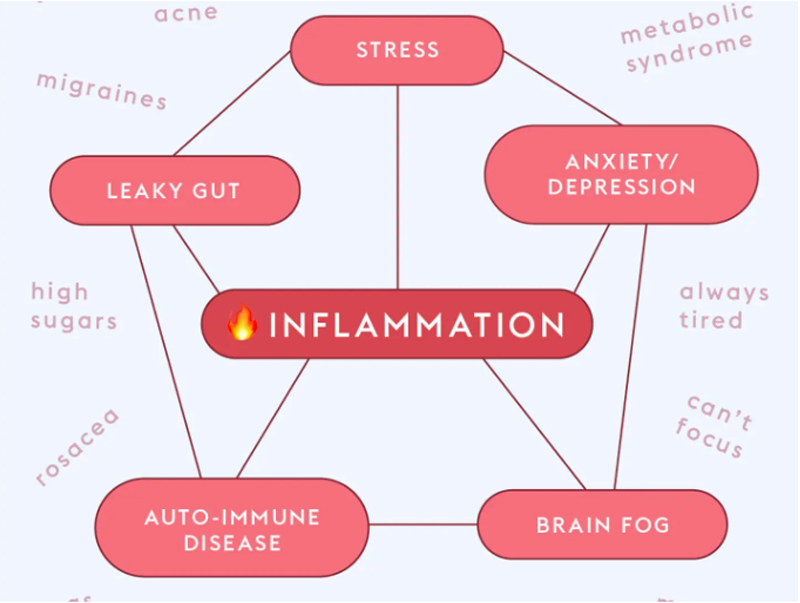
The Ironic thing with inflammation is we might not feel anything developing until it becomes a full-blown, obvious disease.When healthy, properly-functioning cells and the nervous system become dysfunctional, it leads to inflammation. The body ‘s give us prewarning by developing early symptoms of ill health
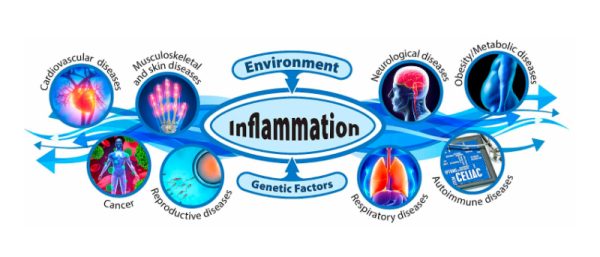
Social, environmental, lifestyle risk factors contributing to Inflammatory cascade:
Physical activity
When skeletal muscles contract, they release proteins that can systematically reduce inflammation.These movement depends on proper development of series of primitive and postural reflexes which can be altered either through an injury during childhood or later in life.Any form of trauma initiates inflammatory cascade through hypoxia or interruption in oxygen flow in the blood and into the tissues.
Developmental origins
Childhood obesity, psychological stress, Physical trauma, Genetic variations, Compromised primitive and postural reflexes, microbial exposure in infancy, and prenatal conditions, inherited health challenges are linked to changes related to inflammation, often through epigenetic changes.
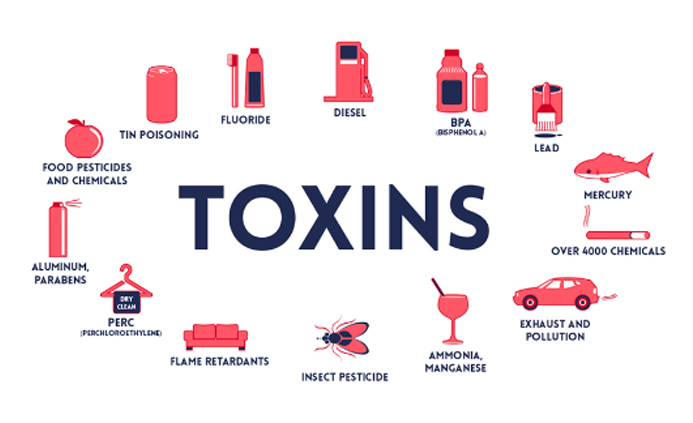
Environmental and industrial toxicants
The federal Tox21 Program in USA has demonstrated that chemicals we commonly encounter alter molecular signaling pathways that underlie inflammation.
Diet
Diets high in refined grains, alcohol, and ultra-processed foods can alter gut microbiota and lead to intestinal , hormonal and immune changes.
Social and cultural changes
Disrupted sleep patterns, psychosocial stress, artificial light, and other factors influence the immune system.
Microbiome
Studies of various microbiome imbalances and disease states show connections to inflammation.
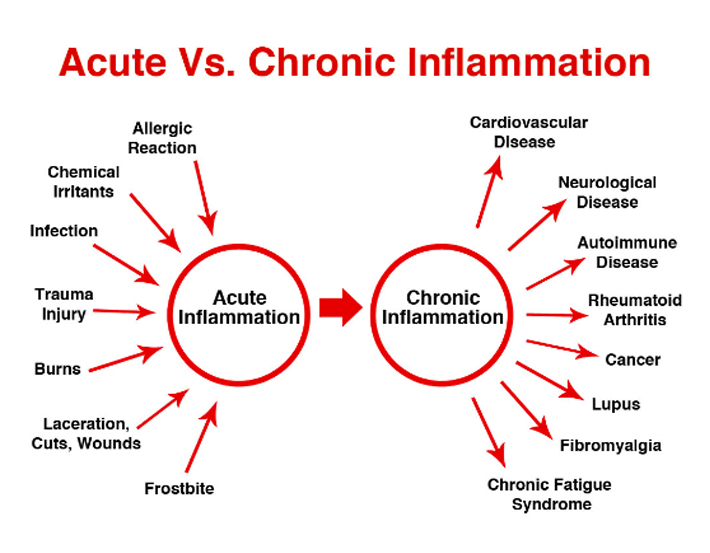
There are generally two types of inflammation: acute and chronic inflammation
Acute Inflammation
Chronic Inflammation
Biochemical contributors to Inflammation:
Low Blood Oxygen Triggers Histamine & Mast Cell Inflammation
Hypoxia, or a state of low oxygen in the body, causes histamine to be released from mast cells. If we’re already dealing with an excess of histamine due to low levels of the histamine degrading diamine oxidase (DAO) enzyme, exposure to high histamine foods, stress, chemical exposure, or illness and injury; avoiding this lack of oxygen to cells is paramount. Low blood oxygen has many causes, including lack of nutrients, stress, not breathing correctly (while awake or asleep), and inflammation. Symptoms include: Shortness of breath, Rapid breathing, Fast heart rate, Low blood pressure, Confusion , Fatigue, poor hormonal regulation, poor sleep, cognitive decline. our mitochondria( the cell’s power engine) require oxygen to produce energy.
There Are Four Types Of Hypoxia or low blood oxygen
- Hypoxic: where there’s not enough oxygen available .
- Hypoxemic: where cells in the body are unable to carry enough oxygen
- Histoxic: where cells are unable to carry enough oxygen because they’re impaired by alcohol or chemicals/drugs
- Stagnant: too little oxygen due to external forces (like being in a fighter jet)
A voluminous amount of research tells us that Low blood oxygen is a driving factor in many chronic diseases.
Interestingly, a study published in the journal Frontiers of Immunology found that the release of histamine in states of low oxygen actually prevents “uncontrolled degranulation” of mast cells (the process by which they release histamine). This stops the body from descending into a state of all out inflammation.
HOW DO WE APPROACH :YOUR HEALTH CONCERNS
Our approach is based on prevention and neuroplasticity. We aim to identify the primary contributing factor of stress leading to activation of inflammatory cascade causing the client’s presenting complaint ( ill health) .
References:
- Furman D, Campisi J, Verdin E, Carrera-Bastos P, Targ S, Franceschi C, Ferrucci L, Gilroy DW, Fasano A, Miller GW, Miller AH, Mantovani A, Weyand CM, Barzilai N, Goronzy JJ, Rando TA, Effros RB, Lucia A, Kleinstreuer N, Slavich GM. 2019. Chronic inflammation in the etiology of disease across the life span. Nat Med 25(12):1822–1832.
- PhD, Charles Patrick Davis MD. “Hypoxia vs Hypoxemia:.MedicineNet. N.p., n.d. Web. 26 July 2017.
- Front. Neurol., Volume 9 – 2018 | , Autonomic Nervous System and Stress https://doi.org/10.3389/fneur.2018.00090
- Liu YZ, Wang YX, Jiang CL. Inflammation: The Common Pathway of Stress-Related Diseases. Front Hum Neurosci. 2017 Jun 20;11:316. doi: 10.3389/fnhum.2017.00316. PMID: 28676747; PMCID: PMC5476783
Breanne E. Kearney1* and Ruth A. Lanius, The brain-body disconnect: A somatic sensory basis for trauma-related disorders, Front. Neurosci., 21 November 2022 Volume 16 – 2022